A cornerstone of modern medicine
Historical context of our work in the evolution of modern transfusion medicine
1901-1907
Blood groups discovered
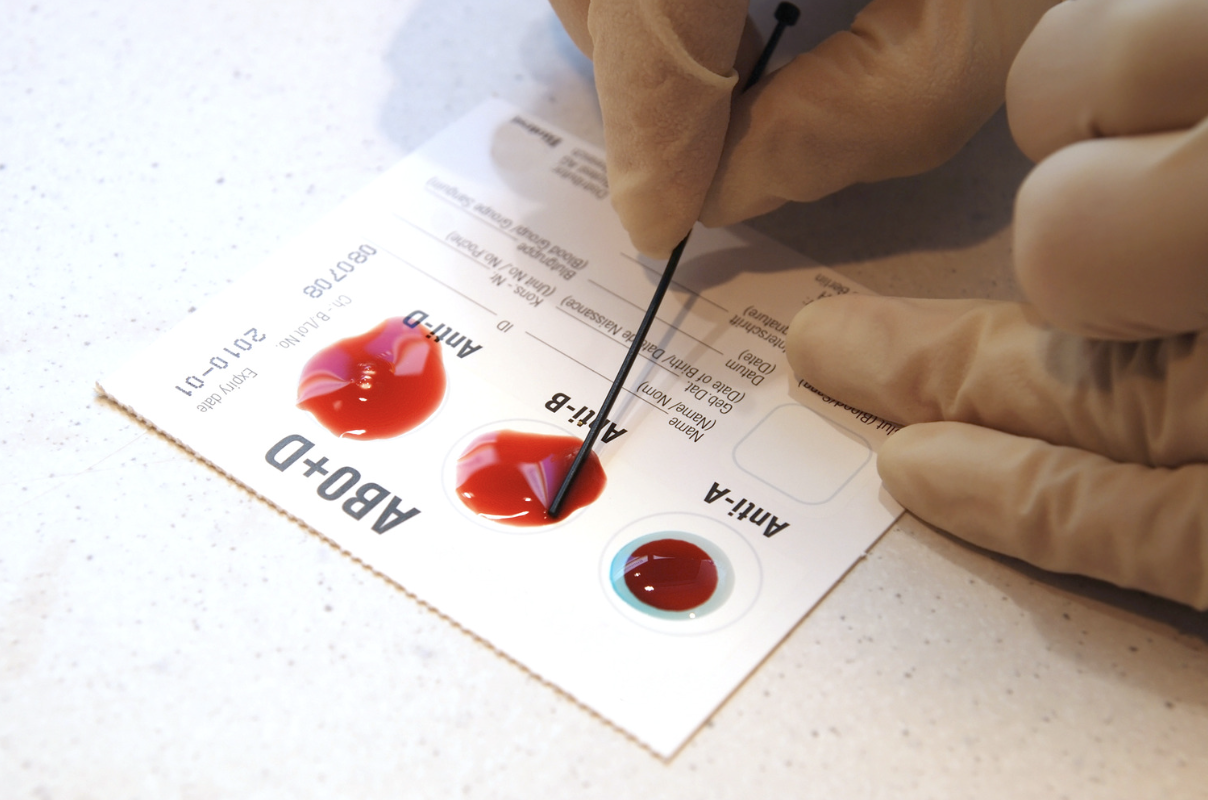
In 1901, Viennese pathologist Karl Landsteiner discovered the ABO blood group system, earning the Nobel Prize in 1930 for this breakthrough. In 1902, Alfred von Decastello and Adriano Sturli identified the fourth major blood group, AB. By 1907, Ludvig Hektoen proposed the crossmatch test to exclude incompatible blood combinations. Following this, Reuben Ottenberg recognized Mendelian inheritance patterns and established that blood group O can serve as a universal donor. In 1925, Karl Landsteiner, along with Phillip Levine, discovered three more blood groups: N, M, and P.
1914-1915
Early advancements in blood preservation
In 1914, Luis Agote of Rawson Hospital in Buenos Aires successfully used citrated blood for preservation on 9 November. The following year, in 1915, Richard Lewisohn of Mount Sinai Hospital in New York successfully used sodium citrate as an anticoagulant, eliminating the need for a direct blood transfusion from donor to recipient.


1940-1946
Development of blood plasma fractionation
In 1940, an interdisciplinary working group of chemists, physists, and physicians developed a method for separating blood plasma into fractions that made components such as albumin, gamma globulin, and fibrinogen available for clinical use. The Cohn extraction method was published in 1946 by Edwin J. Cohn and L. E. Strong. Originally a batch process, it was later developed into a continuous process that significantly improved the efficiency and availability of these vital components for medical treatments.
1985-1999
Advances in blood safety testing
The introduction of the first HIV tests for blood donations in 1985 marked a significant step in making blood transfusions safer. In 1987, two tests for Hepatitis B were developed, followed by the first Hepatitis C test in 1990. By 1992, donor blood was routinely tested for HIV-1 and HIV-2 antibodies. Finally, in 1999, the nucleic acid amplification technique (NAT) was implemented, allowing direct detection of HCV and HIV, significantly enhancing the safety of blood transfusions.


1991-2006
Haemovigilance databanks established
In the early 90's, France and the United Kingdom pioneered European haemovigilance efforts by establishing the Centre National hemovigilance and the SHOT database. In Sweden and Denmark, SCANDAT compiled 34 years of data from 15 million donations and 12 million transfusions. The PROTON study in the Netherlands collected data from 20 hospitals, covering over 2.4 million blood product transfusions for 290,043 patients. This data provided unprecedented insight into the risks and safety of blood transfusion and donation and highlighted the unmet scientific and clinical need to further improve transfusion medicine.
2011
Patient Blood Management (PBM)
Patient Blood Management (PBM), founded in 2011 by Kai Zacharowski and Patrick Meybohm, aims to optimise patient preparation for surgery and minimise blood loss during hospitalisation. Recognising that pre-operative anaemia significantly increases the risk of complications and mortality, PBM strategies include pre-operative anaemia screening and anaemia treatment, often with iron supplements to increase blood production. Blood-saving techniques are used during and after surgery, such as ensuring proper blood clotting and reuse of wound blood. This reduces the need for donor blood, promotes the patient's recovery and conserves vital blood resources.

2024
Registry for the Research of Blood Donor and Recipient Long-Term Outcomes (LOS)
Established in 2024, the LOS registry will track the long-term impact of blood donations and transfusions on patients. This comprehensive, patient-centred study will monitor health outcomes over 30 years and provide valuable data on the long-term impacts. By collecting standardised and high quality patient-level longitudinal data, the registry will support research that improves transfusion practices, enhances patient care and informs health policy. The LOS registry will represent a significant step forward in understanding and improving the safety and efficacy of transfusion and blood management in the future.
Join the LOS Registry Study
Will you continue the journey with us?
How to join our registry study
Explore our multi-stakeholder ecosystem
Get familiar with our forms and documents
Registry Study for Research of Blood Donor and Recipient Long-Term Outcomes
The latest news, articles, and resources on transfusion medicine – follow our deputy study director, Dr Jan Kloka, on LinkedIn.
Address
Universitätsklinikum
Frankfurt am Main
KAIS – Haus 13a
Theodor-Stern-Kai 7
60596 Frankfurt am Main
Contact
© Copyright 2024 by transfusionregistry.org